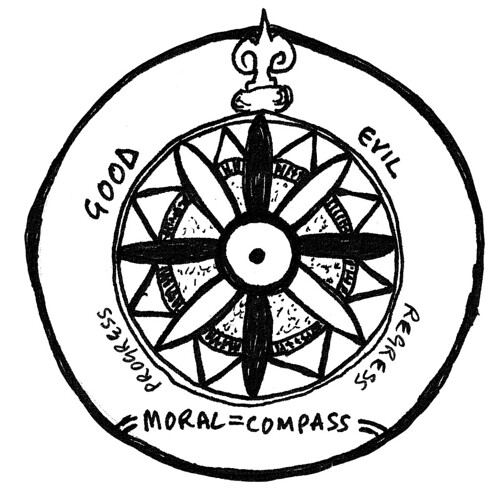
I've been meaning to write a post about how I see different kinds of social networks fitting together and was thinking about how to structure it when lo and behold Harold Jarche linked to this post on his own blog this morning. I've posted his model above.
When I started blogging and tweeting in 2008 my aim was to find other people interested in medical education to connect with. I found some but from the start my external networks have been much more diverse and therefore fruitful that if they were just made up of people interested in people interested in medical education. These are the yellow networks in the diagram above.
Since I was appointed academic lead for eLearning in the medical school in Cardiff University, I have felt the need to try and develop a community of practice with those in similar positions in medical schools acoss the UK. So I started a LinkedIn group called eLearning in Medical Education- not very original! I knew that many of the people who I wanted to join this group were not yet on Twitter or blogging. And I thought that we needed a space that would allow threaded conversation. A few years ago I might have set up a Ning - but this would now cost me £36/year and I don't think it is a format that people are very familiar with in any case. On the other hand, LinkedIn is a social network which those who are aware of it know is work related. So far there are more than 50 members of the group with a reasonable representation of medical schools across the UK. A few medical students have also joined and made some great contributions. I set up a few polls eg Which VLE are you using in your medical school so that newcomers had very non-threatening ways of joining in. And so far the group has been very useful to me at least! It is too early to say that it is a community of practice but it is developing.
And then there are the tools that I use the project teams I am part of within the university. In Cardiff University we have access to IBM connections, a social business solution. The latest version is about to be rolled out. I am going to attempt to use this to share task, project management, information, ideas and developments with all those throughout the university, and in the medical school in particular, who are interested in how we are using technology in the existing course and as we approach a new curriculum.
There has been a lot written recently about the failure of internal networking platforms. A post in the Harvard Business Review last week suggested there is no simple explanation for the poor uptake of internal social networking platforms compared to informal social networking like Twitter and Facebook. A multitude of factors might be responsible including "investing in technology with no clear intent or use in mind" (but who knew why they were signing up to Facebook or Twitter when they fist did? and do all of those corporate accounts know why they are there?). The comments are also well worth reading. One of my favourite comments is the first one "Information flow among desk-sized fiefdoms is usually not free. Attempts to lower the price are almost always met with resistance." The reason that people don't attempt new ways of working is because the cultures of the organisations that they are working within do not give them messages that this is supported and valued. But this intransigence is being challenged by an increasing emphasis on social approaches external to the organisation, and the realisation that to be, as Lee Bryant says, 'social on the outside' also needs good connections and the free flow of information on the inside.
What does 'social on the outside' mean for a university? Who should we be relating to externally as an organisation and as individuals, and as a medical school specifically? Most of the posts on this blog,and the links here, are about me relating externally to other researchers, educators, medical students and patients and a public across the UK and the world. If as educators we are to help students develop digital literacies then we need to consider how these literacies fit with our own identities as researcher and academics and health professionals. And internal social networking platforms may be a safe place to explore identity and utility.
If health organisations also actively engage with 'social on the inside' solutions then perhaps this may impact on how the NHS engages with the use of social media externally. Perhaps.
Do the organisations that you work within provide you with the spaces you need to work with others effectively? Do you think that internal social networking platforms are a waste of time? And is social over-hyped?
EDIT: 24/2/3012 It is really work checking out this post by lecturer in digital media Dr Kelly Page, a colleague in Cardiff University, on "Social Ways of Working in Higher Education".
EDIT: 24/2/3012 It is really work checking out this post by lecturer in digital media Dr Kelly Page, a colleague in Cardiff University, on "Social Ways of Working in Higher Education".